Quick Links
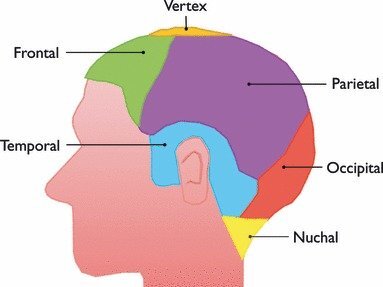
Anatomic Regions of the Scalp
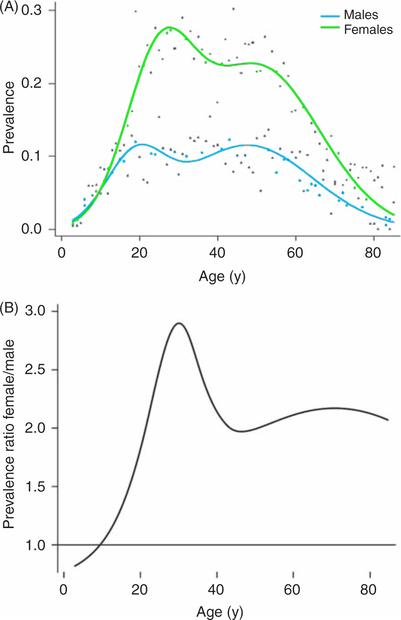
Migraine prevalence by age and sex in the United States
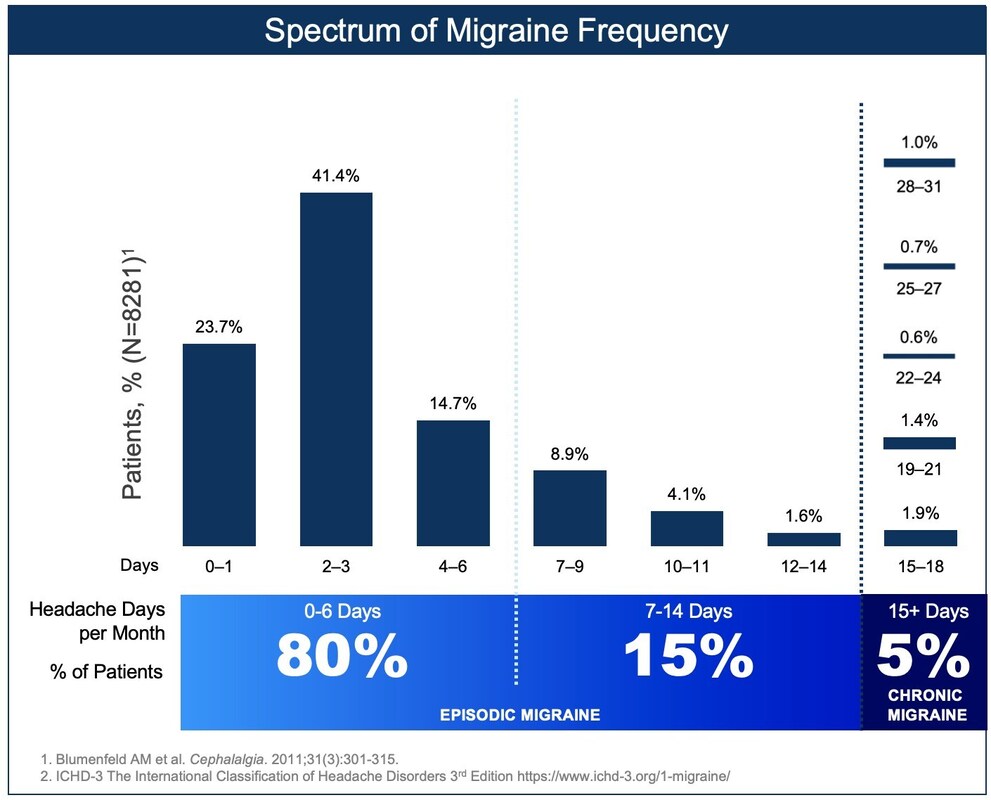
Migraine Frequency
Antidepressants
Amitriptyline
- Adverse effects include anticholinergic effects (eg, dry mouth, urinary retention, constipation), sedation, weight gain, orthostatic hypotension, and cardiac conduction abnormalities.
- Amitriptyline should not be given concomitantly with monoamine oxidase inhibitors, since this may cause serotonin syndrome.
- Drug of choice for Interstitial cystitis/bladder pain syndrome (IC/BPS), chronic bladder pain or discomfort.
- Coadministration with drugs that inhibit cytochrome P450 (eg, selective serotonin inhibitors, cimetidine, many anticonvulsants) should be avoided as they may increase serum levels and result in toxicity.
Venlafaxine (Effexor)
- Venlafaxine XR 150 mg (this dose was used in double-blind trials against amitriptyline 75 mg/day - no difference in efficacy). Can go up to 300 mg/day, even in elderly.
- Weight loss, as effective as amitriptyline; may cause insomnia and also anxiety/nervousness; AEs: nausea, vomiting, drowsiness. Slight BP increase.
- Insomnia and agitation
- Tim Hain uses low dose: Venlafaxine XR 37.5, 1/3 capsule q am for first week, increase to 2/3 capsule for second week, take full capsule from third week on.
- Reduces hot flashes in menopause.
Antidepressants Safe to Use in Elderly
The selective serotonin reuptake inhibitors (SSRIs) and the newer antidepressants buproprion, mirtazapine, moclobemide, and venlafaxine (a selective norepinephrine reuptake inhibitor or SNRI) are all relatively safe in the elderly. They have lower anticholinergic effects than older antidepressants and are thus well tolerated by patients with cardiovascular disease.
Chronic Tension-type Headache
(also metoclpromide increases absorption of other meds)
Herbal and OTC Remedies
Butterbur
Magnesium
Magnesium citrate better absorbed, see below. Magnesium glycinate less diarrhea.
Verapamil
There is weak evidence to support verapamil (Calan) as a first-line agent. Of three small trials comparing verapamil 240 or 320 mg per day with placebo, two reported positive findings.
According to Tim Hain, the usual dose of verapamil is 120 to 240 mg, SR. It takes about 2 weeks to work. The dose may need to be escalated as high as 480 mg/day. Effective in migraine variants such as hemiplegic migraine. Verapamil also may be helpful in Menieres disease. About 50% of users of verapamil develop mild constipation, which can be counteracted by magnesium supplements (500 mg/day). Sometimes verapamil lowers blood pressure but this is generally not a big problem if it is started gradually. About 1% of users develop palpitations. A few individuals develop swelling of the ankles. Because of studies suggesting increased mortality from heart disease, verapamil and related drugs in the calcium channel blocker family are not favored in individuals aged 55 and older. Verapamil increases blood levels of simvistatin. Doses of simvistatin should be reduced to 10 mg when verapamil is also prescribed. Statins also increase the bioavailability of verapamil, and when a statin and verapamil are combined, doses of verapamil should also be decreased.
Amlodipine
According to Alexander Mauskop, amlodipine (Norvasc) has been reported prevent migraine, but reports include a small number of patients. Since verapamil has been studied more extensively, it is usually used first. However, if verapamil works well but causes constipation, which can be severe, can switch to amlodipine. Amlodipine is less likely to cause constipation, but both drugs can cause swelling of the ankles, dizziness and other side effects.
Beta Blockers
Side effects of beta blockers: Fatigue, Bradycardia, Dizziness, Depression, Impotence, Bronchospasm, Nausea (adverse effects are less frequent than with the other first-line agents). Weight gain.
Precautions: Asthma, Chronic heart failure, Diabetes mellitus, Peripheral vascular disease, Conduction defects or heart block, Depression, Raynaud's disease, Hypotension
Special indications: Concurrent hypertension, Angina, Post myocardial infarction, Tremor, Anxiety or panic attacks (specifically propranolol)
Taper beta blockers to avoid withdrawal symptoms.
Metoprolol (Lopressor, Toprolol)
beta1-selective (cardioselective)
50 mg bid; alternatively, metoprolol succinate tablet, extended release (100 mg) at bedtime
Some studies used 200 mg/day.
Propranolol LA
Initial dose should be low (20 mg/day in evening);increase slowly to 60 mg/day adverse effects can occur prior the prophylactic effects and impair patient compliance. Maintained minimum of 3 months to allow efficacy evaluation. When successful prophylactic treatment should be continued for 12 months. Thereafter, discontinuation can be attempted but drug doses should be decreased slowly, particularly with β-adrenoceptor blockers in order to avoid tachycardia or hypertension. The natural history of migraine should then be assessed for 2–3 months.
Nebivolol (Bystolic)
Low side effects
Zyprexa, candesartan cilexetil (16 mg daily)
Namenda (memantine) -10-20 mg/day in divided doses)
Tizanidine (see below for doses)
Atenolol (50 mg daily), olanzapine (2.5-35 mg daily), methylergonovine maleate (0.2-0.4 mg tid),
Zonisamide (Alan Rapoport uses up to 300 mg/day; 400 mg/day is what the package insert says is the maximum useful does in epilepsy although up to 600 mg/day is tolerated)
Chung JY, Kim MW, Kim M. Efficacy of zonisamide in migraineurs with nonresponse to topiramate. Biomed Res Int. 2014;2014:891348. Patients switched to 100 mg/day zonisamide. Low incidence of side effects.
Flunarizine (Sibelium)
10 mg/day (5 mg bid)
My review indicates that it is not less effective than propranolol or topiramate. Canadian Headache Society: Weak recommendation, high quality evidence:While there is high quality evidence that flunarizine 10 mg per day is effective for migraine prophylaxis, a weak recommendation was made because treatment is often limited by side effects, including depression and weight gain.
Flunarizine can be ordered through many online Canadian pharmacies. Patients require prescription.
Rob Cowan: love flunarizine. I use it quite a bit in this setting. Start at 5 mg and go to 10 if necessary. It is very well tolerated in my experience, and pretty damned effective. Nimodipine is also good, but if nicardipine dropped her pressure, I suspect Nimotop will too. Just FYI, the way I prescribe Flunarizine is I write the script and have the patient fax it to CanadaPharmacy. (acquired stereotyped hemiplegic migraine events (following a hypoxic/anoxic event).
Candesartan
Nifedipine can be given prophylactically to avoid MAOI-induced hypertensive crisis. Also, sublingual 10-mg dose of nifedipine can be given and repeated after 20 min.
MAOIs should not be used by persons with thyrotoxicosis or pheochromocytoma.
Abrupt cessation of regular doses of MAOIs can cause a self-limited discontinuation syndrome consisting of arousal, mood disturbances, and somatic symptoms. Doses should be gradually tapered over several week.
MAOIs may lower blood glucose; artificially raise urinary metanephrine; may cause false positive test results for pheochromocytoma or neuroblastoma. Minimal false elevation in thyroid function test resuts.
Phenelzine (Nardil)
This MAO inhibitor (MAOI) is a powerful migraine and daily headache preventive medication. Phenelzine may be used alone, or in combination with amitriptyline, verapamil, or propranolol. Phenelzine is very helpful for depression, anxiety, and panic attacks. The risk of a hypertensive crisis is small but is a major drawback to the MAOIs. Dietary restrictions render MAOIs difficult for the patient. Side effects include insomnia and weight gain, both of which are often major problems. Dry mouth, fatigue, constipation, and cognitive effects may also occur. Patients need to be aware of the symptoms of hypertensive reactions. The usual dose is 45 mg. each night (3 of the 15 mg. tablets). This is adjusted up or down, and the range varies from one to five tablets per day.
Adding beta blocker to MAOI reduces side effects (Merkangas & Merikangas, 1995):
The efficacy of the MAO-I, both alone and in combination with atenolol, was striking. The similarity to the results of previous studies confirms the conclusion of Daroff and Whitney (1986) and others that the MAO-Is may be the most effective treatment for migraine. In the present study, the beneficial effect of the MAO-I was observed for migraine as well as for depression and anxiety. Although the combination of the MAO-I and beta-blocker was not superior to that of the MAO-I alone, beta-blocker permitted subjects with MAO-I-induced side effects of hypotension and hyperarousal to continue treatment with the MAO-I. The mean dose of phenelzine at the end of the study period was 52 mg with a range of 45-75 mg.
(Merikangas KR, Merikangas JR. Combination monoamine oxidase inhibitor and beta-blocker treatment of migraine, with anxiety and depression. Biol Psychiatry. 1995 Nov 1;38(9):603-10. PubMed PMID: 8573662)
EMSAM (selegiline) patch
Can use 3 mg. There are no dietary restrictions on the 6 mg dose of Emsam but higher doses (9 and 12 mg) have not been adequately studied to be confident about the absence of potential for dietary ineractions. Can use in combination with triptans up to 6 mg.
pheneylzine (NARDIL) (nonselective, irreversible MAOI) - may be more effective, EMSAM (selegiline transdermal system) (MAO-B) -may not be effective,
Triptans
Sumavel DosePro SUMATRIPTAN NEEDLE-FREE INJECTION
Sumatriptan injection 6 mg s.q. (0.5 mL)
Cluster: effective (no improved outcome with 12 mg dose in company study)
PK: Time to peak 12 min (range, 6-20 min)
works 5-15 min (a good dose for cluter is 6 mg sumatriptan s.q. with needle)
ALSUMA Auto-Injector SUMATRIPTAN
(US WorldMeds but manufactured by Meridian Medical, Columbia owned by King Pharmaceuticals)
6 mg (can give second injection but no evidence that it is beneficial)
Sumatriptan Nasal Spray
ZOMIG zolmatriptan nasal spray
(Physicians Total Care, Inc.)Sumatriptan Nasal Spray 20 mg (NDC 54868-6052-0) are each supplied in boxes of 6 nasal spray devices. Each unit dose spray supplies 20 mg, respectively, of sumatriptan.
spray is 5 mg, two sprays into each nostril is 10 mg (may repeat for a maximum of 20 mg; higher doses don't give any added benefit)
Intranasal Triptains -- sumatriptan causes metallic/bitter taste; use Zomig (zolmitriptan), 5 mg into one nostril (5 mg/spray), may repeat after 2 h (maximum 10 mg/24 h) (good in teens)
Zomig (zolmatriptan) and Maxalt (rizatriptan) are sold in “melt” formulations
Alan Rapoport says that naratriptan (Amerge, Naramig) 2.5 mg is useful for those who can't tolerate triptans.
Daily NSAIDS (may cause MOH and have side effects, so use cautiously): Celebrex, diclofenac sodium.
Decrease ICP
DHE - Intravenous Treatments
(subcutaneously to prevent nausea) start with 0.5 mg and work up to 1 mg tid (use lower doses > age 50)
use caution in hypertension; Do not use in patients with peripheral vascular disease or heart disease
Don't forget metocloprimide with DHE: Reglan 5 or 10 mg IVP; Metoclopromide p.o. 25 mg or 50 mg;
Solumedrol i.v.; Dexamethasone p.o. 4 mg; Toradol (ketorolac); Give i.v. 60 mg
Clonidine to prevent opiate withdrawal:
(can also use tizanidine; less antihypertensive effect)
TTS #1 patch (0.1 mg)
Clonidine 0.1-0.2 mg PO Q 4-6 hours PRN or by transdermal patch (clonidine transdermal 0.1 mg/24hour patch which provides 0.1 mg a day for 7 days) can be used to treat autonomic hyperactivity symptoms. It will not relieve insomnia. The major drawback of clonidine therapy is the tendency to cause hypotension in some patients. Other agents used for control of withdrawal symptoms include: diphenoxylate/atropine (Lomotil), hydroxyzine, trazodone, and dicyclomine hydrochloride (Bentyl).
Auras without Headache
Generally don't require treatment. Isoproterenol inhaled (beta agonist) may shorten the aura. Sublingual nitroglycerin if need to terminate symptoms rapidly.
Rapid acting NSAIDs meclofenamat or naproxen can be used.
DO NOT USE TRIPTANS.
When to use steroids:
Alan Rapoport: I have often used dexamethasone in a variety of ways. I use it after triptan failures, acutely. I use it for status migrainosus. I use it to help during detoxification if needed. I do not need high doses. 4-8 mg of dexamethasone a day either stat or tapering over 3 days usually does it. Sometimes I use it to break or suppress a cluster period.
Alan Rapoport - 3day steroid taper: dexamethasone 4 mg po tid on Day 1, bid on Day 2 and qd on day 3. You could go a bit longer if you have to. Note: Even though Rapoport does tid dosing, dexamethasone later in the day can cause insomnia.
Alan Rapoport later: Decadron 10 mg IM. Then I give 0.75 mg sig 2 tabs bid X 2 days, 1 tab bid X 2 days, then 1 tab qd X 2 days Alan M. Rapoport, M.D.
A way to do steroid taper with Medrol dose pack: Methylprednisolone 4 mg X 21. Day one 6 tabs, day 2, 5 tabs, etc. (Alan Rapoport says this is too long)
======================================
CLUSTER I think lithium is a reasonable drug to try and the doses useful for cluster are not that big and don't usually require serum monitoring (Lithium carbonate 300 mg at 9 am and 5 pm). Also, I've never found verapamil to be a very good blood pressure medication but it is quite good for cluster and I might consider 80 mg tid along with the lithium and again, keeping a close eye on the blood pressure.
======================================
Migraine/Headache Recipes i.v. DHE (subcutaneously to prevent nausea) start with 0.5 mg and work up to 1 mg tid (use lower doses > age 50) use caution in hypertension; Do not use in patients with peripheral vascular disease or heart disease
Beta Blockers
Metoprolol - 200 mg/day; no AEs
Propranolol - side effects: drowsiness, sleep disturbance, weight gain, fatigue, dry mouth
Side Effects of Beta-Blockers (Medical Letter Jan 2012)Fatigue, depression, bradycardia, erecticle dysfunction, decreased exercise tolerance, heart failure, worsening of peripheral aterial insufficiency, may aggravate allergic reactions, bronchospasm, may mask symptoms of and delay recovery from hypoglycemia, Ranaud's phenomenon, insomnia, vivid dreams or hallucinations, acute mental disorder, increased serum triglycerides, decreased HDL cholsterol, increased incidence of diabetes, sudden withdrawal may lead to exacerbation of antina and mycoardial infarction
New Daily Persistent Headache (NDPH)
Rapid development (over less than 3 days) of an unrelenting headache. Most sufferers can recall the exact day the headache started and have experienced daily headache since that time.
NDPH typically occurs in a person with no past history of headache. MRI with and without enhancement and MRA. These are done to rule out other conditions such as the spontaneous CSF leak) and cerebral venous sinus thrombosis. If these tests are negative, Goadsby et al. recommend considering a LP to rule out infection as well as conditions related to CSF pressure such as idiopathic intracranial hypertension, which can also mimic NDPH.
=======================================================================
Tapering Preventives - Rob Cowan
I keep my patients on a preventive (whether it is Topamax, Verapamil, BOTOX, whichever) for at least three months after they are doing well by their own assessment. If they are doing well subjectively AND they have made the lifestyle changes and behavioral changes, I will taper and d/c the preventive. I will then follow them with a calendar to monitor medication use and headache frequency, etc. I have always viewed preventives as a tool that allows the patient enough respite to make the changes sleep hygeine, exercise, eating behaviors and stress mgmt necessary to decrease frequency and severity. That being said, I would say about a third of my patients end up back on a preventive regardless. My best reference for this is a wonderful article by Bigal and Lipton looking at factors contributing to progression from LFEM to CM and back again.Rob ===================================
Propranolol (Beta-Blockers) and sleep: use of Melatonin
CNS Side effects from package insert:Light-headedness; mental depression manifested by insomnia, lassitude, weakness, fatigue; catatonia; visual disturbances; hallucinations; vivid dreams; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics.
Can improved sleep time and sleep efficiency with: 2.5 mg melatonin nightly for 3 weeks
=====================
Intranasal lidocaine
=======================
Chronic daily headache - Secondary causes
Primary chronic headaches of long duration include chronic migraine, chronic tension-type headache, new daily persistent headache, and hemicrania continua.
Secondary headaches that can mimic primary headache types: arteriovenous malformations, spontaneous intracranial hypotension, neoplasms, pseudotumor cerebri, cervical artery dissections, cerebral venous thrombosis, Chiari I malformation, and temporal arteritis.
==========================
Headache Glasses - FL-41 (rose colored; fluorescent light sensitivity)
http://www.headaches.org/2017/03/27/light-headache-disorders-understanding-light-triggers-photophobia/
TheraSpecs
http://www.theraspecs.com/
AxonOptics
https://www.axonoptics.com/
SomniLight
http://www.somnilight.com/
Neuro-Ophthalmology
Article written by Marianne Doran. November/December 2005
Rose-colored sunglasses. Preliminary research at the University of Utah suggests that specially tinted lens may help some people with photophobia. Anecdotally, many photophobic patients prefer an FL-41 tint on their sunglasses instead of green or yellow. The FL-41 tint, which has a pinkish look to it, is a mixture of colors that blocks the blue-green wavelengths.
"We randomized patients with blepharospasm to wearing FL-41 sunglasses for two weeks and then to wearing plain sunglasses for two weeks," said Dr. Katz. "The patients filled out questionnaires at the end of each period. We found that patients with blepharospasm definitely preferred wearing lenses with the FL-41 tint to wearing conventional sunglasses. So there does seem to be some therapeutic benefit."
In a new study, the researchers have used electromyography to measure blink frequency, duration and amplitude in blepharospasm patients while they read for five minutes at a time with regular eyeglasses, glasses with a light gray tint or glasses with an FL-41 tint. The results are still being analyzed, but Dr. Katz said they appear to provide more objective evidence that FL-41 does reduce blepharospasm.
"FL-41 lenses are non-invasive, they have no side effects and they're not expensive," Dr. Katz added. "So it's a cheap, easy way to improve the lives of these patients, who in some cases are very disabled by their disease."
Be sure glasses block blue-green. FL-41 lenses are available in optical shops, but Dr. Digre cautioned that some so-called FL-41 lenses are not the real thing. "You really have to know whether the lenses are real or not." she said. "Some lenses can look like FL-41, but they don't act like it. We have done spectral analysis of our lenses to make sure they are blocking the right light".
=====================================
ADDICTION TREATMENT
Web site to find Addiction Treatment Specialists
Turn to Help (Reckitt Benckiser Pharmaceuticals, maker of Suboxone)
http://turntohelp.com
The selective serotonin reuptake inhibitors (SSRIs) and the newer antidepressants buproprion, mirtazapine, moclobemide, and venlafaxine (a selective norepinephrine reuptake inhibitor or SNRI) are all relatively safe in the elderly. They have lower anticholinergic effects than older antidepressants and are thus well tolerated by patients with cardiovascular disease.
Chronic Tension-type Headache
- Second line: Mirtazepine (Remeron) 15-30 mg/day q hs (somnolence, increased appetite, weight gain; antinausea - 5-HT3 antagonism!!) and venlafaxine
- Tizanidine (up to 24 mg/day, but maximum dose is 32 to 36 mg/day) - used in the treatment of paravertebral muscle spasm in association with acute low back pain; chronic daily headache; detoxification to assist with analgesic withdrawal in patients with analgesic rebound headache. Not as potent as clonidine as antihypertensive
- Amitryptyline (TCAs) decrease REM sleep % but tolerance may develop to REM suppression with a marked rebound following drug withdral
- Mirtazepine: potent 5-HT2 and 5-HT3 antagonist (antinausea); potent H1 antagonist (prominent sedative effects); moderate peripheral α1 adrenergic antagonist, occasional orthostatic hypotension; moderate muscarainic receptor antagonist, may explain low incidence of anticholinergic side effects; does not affect REM sleep % or latency.
(also metoclpromide increases absorption of other meds)
- Metoclopromide [REGLAN] 5 mg; usual dose 10 mg (tardive dyskinesia should only be a problem with chronic use at high doses) (may help with medication absorption
- Promethazine HCl 25 mg (will cause sleepiness) [brand name PHENERGAN], available as injection and as suppository
- Ondansetron HCl 8 mg p.o. (no sleepiness) [can use up to 3 tablets] [ZOFRAN] ondansetron HCl orally disintigrating tablet. I gave ondansetron (Zofran) 4 mg i.m. with good effect for nausea
- Other options: chloropromazine (Thorazine), prochlorperazine (Compazine), trimethobenzamide (Tigan), Hydroxyzine [Vistaril, Atarax] not specifically indicated for nausea but sedative
- Transderm scop patch [behind ear]
Herbal and OTC Remedies
Butterbur
- 75 mg twice a day
- Petadolex (Weber & Weber USA; Orlando, FL) http://www.petadolex.com/default.aspx
- Linpharma Inc., 4368 L.B. McLeod RD, Orlando FL 32811, Toll Free: 1.888.301.1084, Email: CustomerService@petadolex.com
- Butterbur extract. Must use form that is PA-Free (pyrolizidine alkaloids, which are carcinogenic and cause liver and kidney damage)
- Among the natural treatments, there is good evidence from clinical trials that an extract of the rhizome of the butterbur plant (Petadolex;Weber & Weber USA, Orlando, FL) is effective in reducing the frequency of migraine headaches when administered in divided doses of either 100 mg or 150 mg daily. Class I.
- Safe for children 6-17, Also relieves allergy symptoms.
- Riboflavin 400 mg daily
- Co-enzyme Q10 100
- Boswellia extract
Magnesium
Magnesium citrate better absorbed, see below. Magnesium glycinate less diarrhea.
- The daily recommended dose is 400 mg of magnesium oxide (antacid), magnesium citrate (300 mg twice daily), chelated magnesium (magnesium aspartate, diglycinate, gluconate, etc.)
- Magnesium 600 mg hs, magnesium glycinate and magnesium gluconate, less likely to cause diarrhea (contraindicated in renal failure)
- In one study, 600 mg (24 mmol) magnesium (trimagnesium dicitrate) was effective in migraine prophylaxis but caused diarrhea in 18.6%.
- BEST ? magnesium diglycinate (magnesium glycinate), magnesium taurate (literature limited)
- Magnesium oxide - poor bioavailability (do not use)
- Equivalent bioavailability: magnesium chloride, magnesium lactate, magnesium aspartate, magnesium citrate
- Chloride, sulfate, citrate, lactate, malate, glycinate, taurinate - highly biologically available
Verapamil
There is weak evidence to support verapamil (Calan) as a first-line agent. Of three small trials comparing verapamil 240 or 320 mg per day with placebo, two reported positive findings.
According to Tim Hain, the usual dose of verapamil is 120 to 240 mg, SR. It takes about 2 weeks to work. The dose may need to be escalated as high as 480 mg/day. Effective in migraine variants such as hemiplegic migraine. Verapamil also may be helpful in Menieres disease. About 50% of users of verapamil develop mild constipation, which can be counteracted by magnesium supplements (500 mg/day). Sometimes verapamil lowers blood pressure but this is generally not a big problem if it is started gradually. About 1% of users develop palpitations. A few individuals develop swelling of the ankles. Because of studies suggesting increased mortality from heart disease, verapamil and related drugs in the calcium channel blocker family are not favored in individuals aged 55 and older. Verapamil increases blood levels of simvistatin. Doses of simvistatin should be reduced to 10 mg when verapamil is also prescribed. Statins also increase the bioavailability of verapamil, and when a statin and verapamil are combined, doses of verapamil should also be decreased.
Amlodipine
According to Alexander Mauskop, amlodipine (Norvasc) has been reported prevent migraine, but reports include a small number of patients. Since verapamil has been studied more extensively, it is usually used first. However, if verapamil works well but causes constipation, which can be severe, can switch to amlodipine. Amlodipine is less likely to cause constipation, but both drugs can cause swelling of the ankles, dizziness and other side effects.
Beta Blockers
Side effects of beta blockers: Fatigue, Bradycardia, Dizziness, Depression, Impotence, Bronchospasm, Nausea (adverse effects are less frequent than with the other first-line agents). Weight gain.
Precautions: Asthma, Chronic heart failure, Diabetes mellitus, Peripheral vascular disease, Conduction defects or heart block, Depression, Raynaud's disease, Hypotension
Special indications: Concurrent hypertension, Angina, Post myocardial infarction, Tremor, Anxiety or panic attacks (specifically propranolol)
Taper beta blockers to avoid withdrawal symptoms.
Metoprolol (Lopressor, Toprolol)
beta1-selective (cardioselective)
50 mg bid; alternatively, metoprolol succinate tablet, extended release (100 mg) at bedtime
Some studies used 200 mg/day.
Propranolol LA
Initial dose should be low (20 mg/day in evening);increase slowly to 60 mg/day adverse effects can occur prior the prophylactic effects and impair patient compliance. Maintained minimum of 3 months to allow efficacy evaluation. When successful prophylactic treatment should be continued for 12 months. Thereafter, discontinuation can be attempted but drug doses should be decreased slowly, particularly with β-adrenoceptor blockers in order to avoid tachycardia or hypertension. The natural history of migraine should then be assessed for 2–3 months.
Nebivolol (Bystolic)
Low side effects
Zyprexa, candesartan cilexetil (16 mg daily)
Namenda (memantine) -10-20 mg/day in divided doses)
Tizanidine (see below for doses)
Atenolol (50 mg daily), olanzapine (2.5-35 mg daily), methylergonovine maleate (0.2-0.4 mg tid),
Zonisamide (Alan Rapoport uses up to 300 mg/day; 400 mg/day is what the package insert says is the maximum useful does in epilepsy although up to 600 mg/day is tolerated)
Chung JY, Kim MW, Kim M. Efficacy of zonisamide in migraineurs with nonresponse to topiramate. Biomed Res Int. 2014;2014:891348. Patients switched to 100 mg/day zonisamide. Low incidence of side effects.
Flunarizine (Sibelium)
10 mg/day (5 mg bid)
My review indicates that it is not less effective than propranolol or topiramate. Canadian Headache Society: Weak recommendation, high quality evidence:While there is high quality evidence that flunarizine 10 mg per day is effective for migraine prophylaxis, a weak recommendation was made because treatment is often limited by side effects, including depression and weight gain.
Flunarizine can be ordered through many online Canadian pharmacies. Patients require prescription.
Rob Cowan: love flunarizine. I use it quite a bit in this setting. Start at 5 mg and go to 10 if necessary. It is very well tolerated in my experience, and pretty damned effective. Nimodipine is also good, but if nicardipine dropped her pressure, I suspect Nimotop will too. Just FYI, the way I prescribe Flunarizine is I write the script and have the patient fax it to CanadaPharmacy. (acquired stereotyped hemiplegic migraine events (following a hypoxic/anoxic event).
Candesartan
- 16 mg/day
- Strong recommendation, moderate quality evidence: We recommend that clinicians offer candesartan (16 mg per day) to eligible patients for migraine prophylaxis. Although the evidence that candesartan provides a reduction in migraine frequency is limited, one good randomized trial supports its use and side effects of treatment are minimal. (Canadian Headache Society, March 2012)
- alpha2 agonist - better tolerated than baclofen but can cause hypotension (less than clonidine). Sedative! Need to up titrate slowly. I too have heard patients mention nightmares. The article quoted by Jack, from Saper et al, is a large sample but does contain 77 % migraineurs, the rest being mixed patients.We must keep in mind that tension-type headache as well seems to be sensitive to the drug in a study (although smaller range, female gender only) [Fogelholm R, Murros K. Tizanidine in chronic tension-type headache: a placebo controlled double-blind cross-over study. Headache 1992;32(10):509-13. PMID: 1468911]. This must be kept in mind in "chronic daily headache" even though most are transformed migraine. Marc Lenaerts. Tizanidine is worth a try in chronic migraine or in chronic tension-type headache: Slowly titrate (over 4 weeks) to 24 mg or the maximum dose tolerated (divided t.i.d.). Tizanidine 8 mg tid
Nifedipine can be given prophylactically to avoid MAOI-induced hypertensive crisis. Also, sublingual 10-mg dose of nifedipine can be given and repeated after 20 min.
MAOIs should not be used by persons with thyrotoxicosis or pheochromocytoma.
Abrupt cessation of regular doses of MAOIs can cause a self-limited discontinuation syndrome consisting of arousal, mood disturbances, and somatic symptoms. Doses should be gradually tapered over several week.
MAOIs may lower blood glucose; artificially raise urinary metanephrine; may cause false positive test results for pheochromocytoma or neuroblastoma. Minimal false elevation in thyroid function test resuts.
Phenelzine (Nardil)
This MAO inhibitor (MAOI) is a powerful migraine and daily headache preventive medication. Phenelzine may be used alone, or in combination with amitriptyline, verapamil, or propranolol. Phenelzine is very helpful for depression, anxiety, and panic attacks. The risk of a hypertensive crisis is small but is a major drawback to the MAOIs. Dietary restrictions render MAOIs difficult for the patient. Side effects include insomnia and weight gain, both of which are often major problems. Dry mouth, fatigue, constipation, and cognitive effects may also occur. Patients need to be aware of the symptoms of hypertensive reactions. The usual dose is 45 mg. each night (3 of the 15 mg. tablets). This is adjusted up or down, and the range varies from one to five tablets per day.
Adding beta blocker to MAOI reduces side effects (Merkangas & Merikangas, 1995):
The efficacy of the MAO-I, both alone and in combination with atenolol, was striking. The similarity to the results of previous studies confirms the conclusion of Daroff and Whitney (1986) and others that the MAO-Is may be the most effective treatment for migraine. In the present study, the beneficial effect of the MAO-I was observed for migraine as well as for depression and anxiety. Although the combination of the MAO-I and beta-blocker was not superior to that of the MAO-I alone, beta-blocker permitted subjects with MAO-I-induced side effects of hypotension and hyperarousal to continue treatment with the MAO-I. The mean dose of phenelzine at the end of the study period was 52 mg with a range of 45-75 mg.
(Merikangas KR, Merikangas JR. Combination monoamine oxidase inhibitor and beta-blocker treatment of migraine, with anxiety and depression. Biol Psychiatry. 1995 Nov 1;38(9):603-10. PubMed PMID: 8573662)
EMSAM (selegiline) patch
Can use 3 mg. There are no dietary restrictions on the 6 mg dose of Emsam but higher doses (9 and 12 mg) have not been adequately studied to be confident about the absence of potential for dietary ineractions. Can use in combination with triptans up to 6 mg.
pheneylzine (NARDIL) (nonselective, irreversible MAOI) - may be more effective, EMSAM (selegiline transdermal system) (MAO-B) -may not be effective,
Triptans
Sumavel DosePro SUMATRIPTAN NEEDLE-FREE INJECTION
Sumatriptan injection 6 mg s.q. (0.5 mL)
Cluster: effective (no improved outcome with 12 mg dose in company study)
PK: Time to peak 12 min (range, 6-20 min)
works 5-15 min (a good dose for cluter is 6 mg sumatriptan s.q. with needle)
ALSUMA Auto-Injector SUMATRIPTAN
(US WorldMeds but manufactured by Meridian Medical, Columbia owned by King Pharmaceuticals)
6 mg (can give second injection but no evidence that it is beneficial)
Sumatriptan Nasal Spray
ZOMIG zolmatriptan nasal spray
(Physicians Total Care, Inc.)Sumatriptan Nasal Spray 20 mg (NDC 54868-6052-0) are each supplied in boxes of 6 nasal spray devices. Each unit dose spray supplies 20 mg, respectively, of sumatriptan.
spray is 5 mg, two sprays into each nostril is 10 mg (may repeat for a maximum of 20 mg; higher doses don't give any added benefit)
Intranasal Triptains -- sumatriptan causes metallic/bitter taste; use Zomig (zolmitriptan), 5 mg into one nostril (5 mg/spray), may repeat after 2 h (maximum 10 mg/24 h) (good in teens)
Zomig (zolmatriptan) and Maxalt (rizatriptan) are sold in “melt” formulations
Alan Rapoport says that naratriptan (Amerge, Naramig) 2.5 mg is useful for those who can't tolerate triptans.
Daily NSAIDS (may cause MOH and have side effects, so use cautiously): Celebrex, diclofenac sodium.
Decrease ICP
DHE - Intravenous Treatments
(subcutaneously to prevent nausea) start with 0.5 mg and work up to 1 mg tid (use lower doses > age 50)
use caution in hypertension; Do not use in patients with peripheral vascular disease or heart disease
Don't forget metocloprimide with DHE: Reglan 5 or 10 mg IVP; Metoclopromide p.o. 25 mg or 50 mg;
Solumedrol i.v.; Dexamethasone p.o. 4 mg; Toradol (ketorolac); Give i.v. 60 mg
Clonidine to prevent opiate withdrawal:
(can also use tizanidine; less antihypertensive effect)
TTS #1 patch (0.1 mg)
Clonidine 0.1-0.2 mg PO Q 4-6 hours PRN or by transdermal patch (clonidine transdermal 0.1 mg/24hour patch which provides 0.1 mg a day for 7 days) can be used to treat autonomic hyperactivity symptoms. It will not relieve insomnia. The major drawback of clonidine therapy is the tendency to cause hypotension in some patients. Other agents used for control of withdrawal symptoms include: diphenoxylate/atropine (Lomotil), hydroxyzine, trazodone, and dicyclomine hydrochloride (Bentyl).
Auras without Headache
Generally don't require treatment. Isoproterenol inhaled (beta agonist) may shorten the aura. Sublingual nitroglycerin if need to terminate symptoms rapidly.
Rapid acting NSAIDs meclofenamat or naproxen can be used.
DO NOT USE TRIPTANS.
When to use steroids:
Alan Rapoport: I have often used dexamethasone in a variety of ways. I use it after triptan failures, acutely. I use it for status migrainosus. I use it to help during detoxification if needed. I do not need high doses. 4-8 mg of dexamethasone a day either stat or tapering over 3 days usually does it. Sometimes I use it to break or suppress a cluster period.
Alan Rapoport - 3day steroid taper: dexamethasone 4 mg po tid on Day 1, bid on Day 2 and qd on day 3. You could go a bit longer if you have to. Note: Even though Rapoport does tid dosing, dexamethasone later in the day can cause insomnia.
Alan Rapoport later: Decadron 10 mg IM. Then I give 0.75 mg sig 2 tabs bid X 2 days, 1 tab bid X 2 days, then 1 tab qd X 2 days Alan M. Rapoport, M.D.
A way to do steroid taper with Medrol dose pack: Methylprednisolone 4 mg X 21. Day one 6 tabs, day 2, 5 tabs, etc. (Alan Rapoport says this is too long)
======================================
CLUSTER I think lithium is a reasonable drug to try and the doses useful for cluster are not that big and don't usually require serum monitoring (Lithium carbonate 300 mg at 9 am and 5 pm). Also, I've never found verapamil to be a very good blood pressure medication but it is quite good for cluster and I might consider 80 mg tid along with the lithium and again, keeping a close eye on the blood pressure.
======================================
Migraine/Headache Recipes i.v. DHE (subcutaneously to prevent nausea) start with 0.5 mg and work up to 1 mg tid (use lower doses > age 50) use caution in hypertension; Do not use in patients with peripheral vascular disease or heart disease
Beta Blockers
Metoprolol - 200 mg/day; no AEs
Propranolol - side effects: drowsiness, sleep disturbance, weight gain, fatigue, dry mouth
Side Effects of Beta-Blockers (Medical Letter Jan 2012)Fatigue, depression, bradycardia, erecticle dysfunction, decreased exercise tolerance, heart failure, worsening of peripheral aterial insufficiency, may aggravate allergic reactions, bronchospasm, may mask symptoms of and delay recovery from hypoglycemia, Ranaud's phenomenon, insomnia, vivid dreams or hallucinations, acute mental disorder, increased serum triglycerides, decreased HDL cholsterol, increased incidence of diabetes, sudden withdrawal may lead to exacerbation of antina and mycoardial infarction
New Daily Persistent Headache (NDPH)
Rapid development (over less than 3 days) of an unrelenting headache. Most sufferers can recall the exact day the headache started and have experienced daily headache since that time.
NDPH typically occurs in a person with no past history of headache. MRI with and without enhancement and MRA. These are done to rule out other conditions such as the spontaneous CSF leak) and cerebral venous sinus thrombosis. If these tests are negative, Goadsby et al. recommend considering a LP to rule out infection as well as conditions related to CSF pressure such as idiopathic intracranial hypertension, which can also mimic NDPH.
=======================================================================
Tapering Preventives - Rob Cowan
I keep my patients on a preventive (whether it is Topamax, Verapamil, BOTOX, whichever) for at least three months after they are doing well by their own assessment. If they are doing well subjectively AND they have made the lifestyle changes and behavioral changes, I will taper and d/c the preventive. I will then follow them with a calendar to monitor medication use and headache frequency, etc. I have always viewed preventives as a tool that allows the patient enough respite to make the changes sleep hygeine, exercise, eating behaviors and stress mgmt necessary to decrease frequency and severity. That being said, I would say about a third of my patients end up back on a preventive regardless. My best reference for this is a wonderful article by Bigal and Lipton looking at factors contributing to progression from LFEM to CM and back again.Rob ===================================
Propranolol (Beta-Blockers) and sleep: use of Melatonin
CNS Side effects from package insert:Light-headedness; mental depression manifested by insomnia, lassitude, weakness, fatigue; catatonia; visual disturbances; hallucinations; vivid dreams; an acute reversible syndrome characterized by disorientation for time and place, short-term memory loss, emotional lability, slightly clouded sensorium, and decreased performance on neuropsychometrics.
Can improved sleep time and sleep efficiency with: 2.5 mg melatonin nightly for 3 weeks
=====================
Intranasal lidocaine
- 4% isotonic (saline to make isotonic)
- 30 mL spray bottle
- Davis Compounding Solutions (Chuck) 530-756-1255
- Neil Raskin used to use for migraine
- For cluster: Dripped or sprayed lidocaine (1 mL at concentrations of 4-10%), in the nostril of the symptomatic side, provides quick (within 10 min) improvement to at least one third of the treated patients.27-31 Intranasal lidocaine, however, hardly ever provides complete relief, and thus it can be used as an adjuvant for other abortive treatments. In order to facilitate drug access to pain fibers running through the sphenopalatine ganglion in the retro-orbital area, lidocaine should be instilled with the patient lying in a horizontal position, with the head bent backwards and rotated toward the painful side. After application, this position should be maintained for at least 5 min.
=======================
Chronic daily headache - Secondary causes
Primary chronic headaches of long duration include chronic migraine, chronic tension-type headache, new daily persistent headache, and hemicrania continua.
Secondary headaches that can mimic primary headache types: arteriovenous malformations, spontaneous intracranial hypotension, neoplasms, pseudotumor cerebri, cervical artery dissections, cerebral venous thrombosis, Chiari I malformation, and temporal arteritis.
==========================
Headache Glasses - FL-41 (rose colored; fluorescent light sensitivity)
http://www.headaches.org/2017/03/27/light-headache-disorders-understanding-light-triggers-photophobia/
TheraSpecs
http://www.theraspecs.com/
AxonOptics
https://www.axonoptics.com/
SomniLight
http://www.somnilight.com/
Neuro-Ophthalmology
Article written by Marianne Doran. November/December 2005
Rose-colored sunglasses. Preliminary research at the University of Utah suggests that specially tinted lens may help some people with photophobia. Anecdotally, many photophobic patients prefer an FL-41 tint on their sunglasses instead of green or yellow. The FL-41 tint, which has a pinkish look to it, is a mixture of colors that blocks the blue-green wavelengths.
"We randomized patients with blepharospasm to wearing FL-41 sunglasses for two weeks and then to wearing plain sunglasses for two weeks," said Dr. Katz. "The patients filled out questionnaires at the end of each period. We found that patients with blepharospasm definitely preferred wearing lenses with the FL-41 tint to wearing conventional sunglasses. So there does seem to be some therapeutic benefit."
In a new study, the researchers have used electromyography to measure blink frequency, duration and amplitude in blepharospasm patients while they read for five minutes at a time with regular eyeglasses, glasses with a light gray tint or glasses with an FL-41 tint. The results are still being analyzed, but Dr. Katz said they appear to provide more objective evidence that FL-41 does reduce blepharospasm.
"FL-41 lenses are non-invasive, they have no side effects and they're not expensive," Dr. Katz added. "So it's a cheap, easy way to improve the lives of these patients, who in some cases are very disabled by their disease."
Be sure glasses block blue-green. FL-41 lenses are available in optical shops, but Dr. Digre cautioned that some so-called FL-41 lenses are not the real thing. "You really have to know whether the lenses are real or not." she said. "Some lenses can look like FL-41, but they don't act like it. We have done spectral analysis of our lenses to make sure they are blocking the right light".
=====================================
ADDICTION TREATMENT
Web site to find Addiction Treatment Specialists
Turn to Help (Reckitt Benckiser Pharmaceuticals, maker of Suboxone)
http://turntohelp.com