Nerve Blocks
Most common anesthetics: lidocaine (1%), bupivacaine (0.25% = 2.5 mg/mL)
Lidocaine preferred in pregnancy.
Bupivicaine 0.25% (Marcaine) now available in clinic (8/19/2019)
Marcaine 0.25% (bupivacaine hydrochloride 2.5 mg/mL with epinephrine 1:200,000 as bitartrate)
Lidocaine preferred in pregnancy.
Bupivicaine 0.25% (Marcaine) now available in clinic (8/19/2019)
- 5 mL syringe
- 18 gauge needle
- 1 1/2 inch 27 gauge needle
- alcohol pad or chlorprep
- gloves
Marcaine 0.25% (bupivacaine hydrochloride 2.5 mg/mL with epinephrine 1:200,000 as bitartrate)
Occipital Nerve Block
- Diagnose and treat occipital neuralgia
- Use in headache made worse by palpation of occipital nerve
- Occipital neuralgia
- Cluster headache
- Cervicogenic headache
- Migraine, particularly with occipital nerve irritation or tenderness
- Allergy to medication
- Localized skin reaction or infection
- Injury to occipital artery with hematoma
- Injury to nerve with resultant numbness to scalp or neck
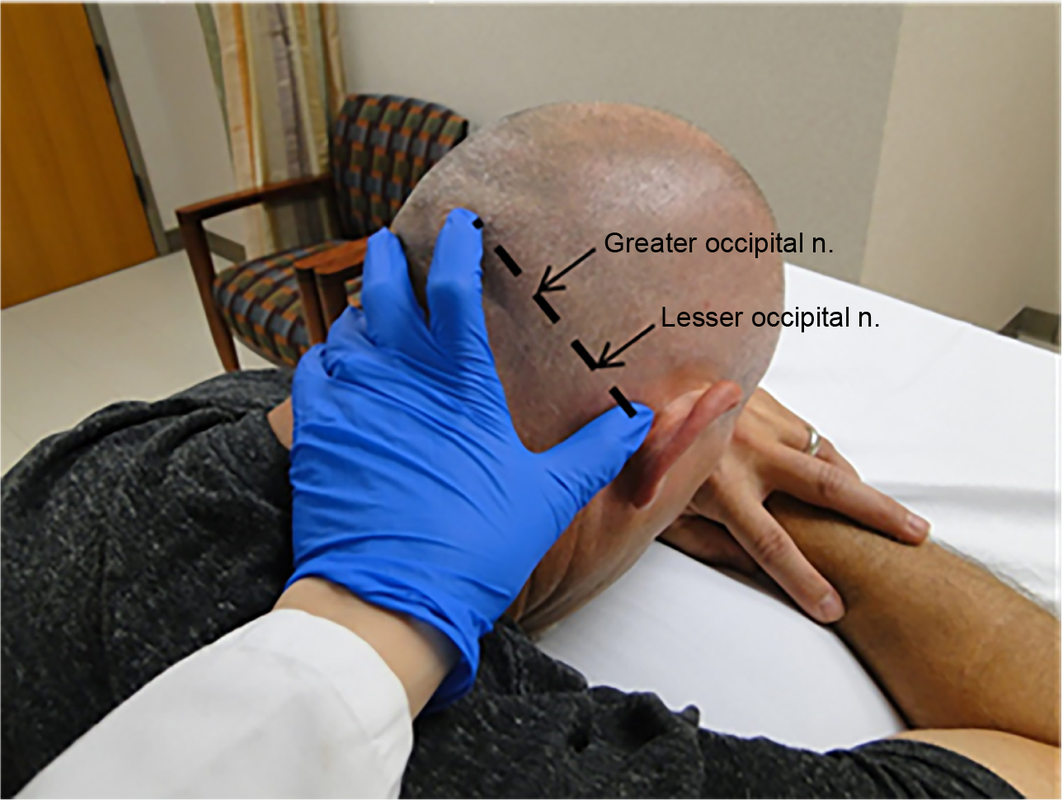
Patient puts face in hands.
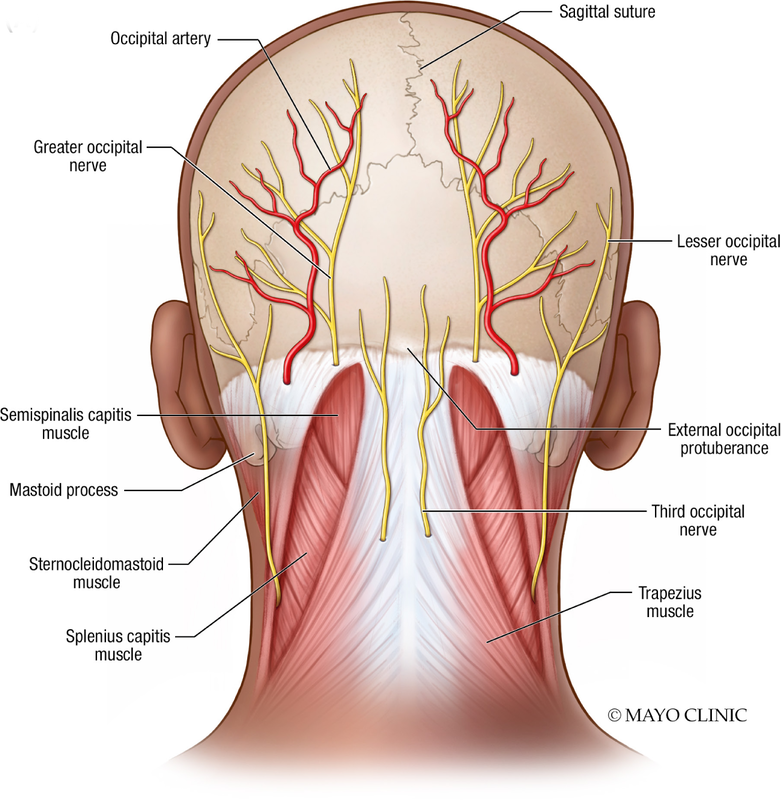
Fan fluid; go lateral to get lesser occipital nerve.
Relief of pain 5 to 10 minutes
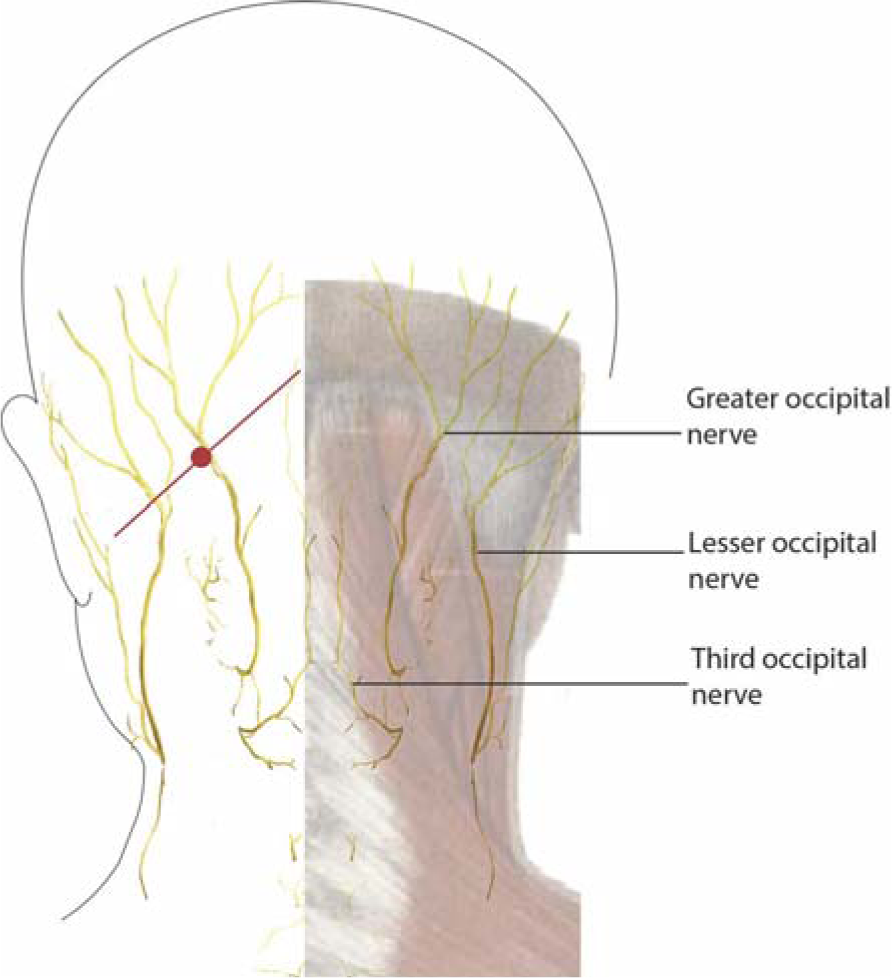
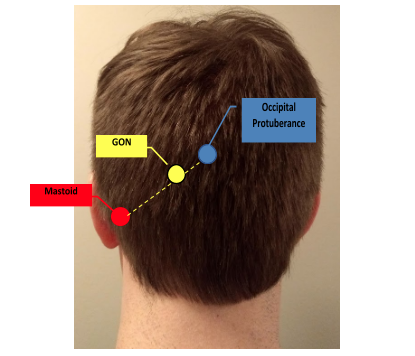
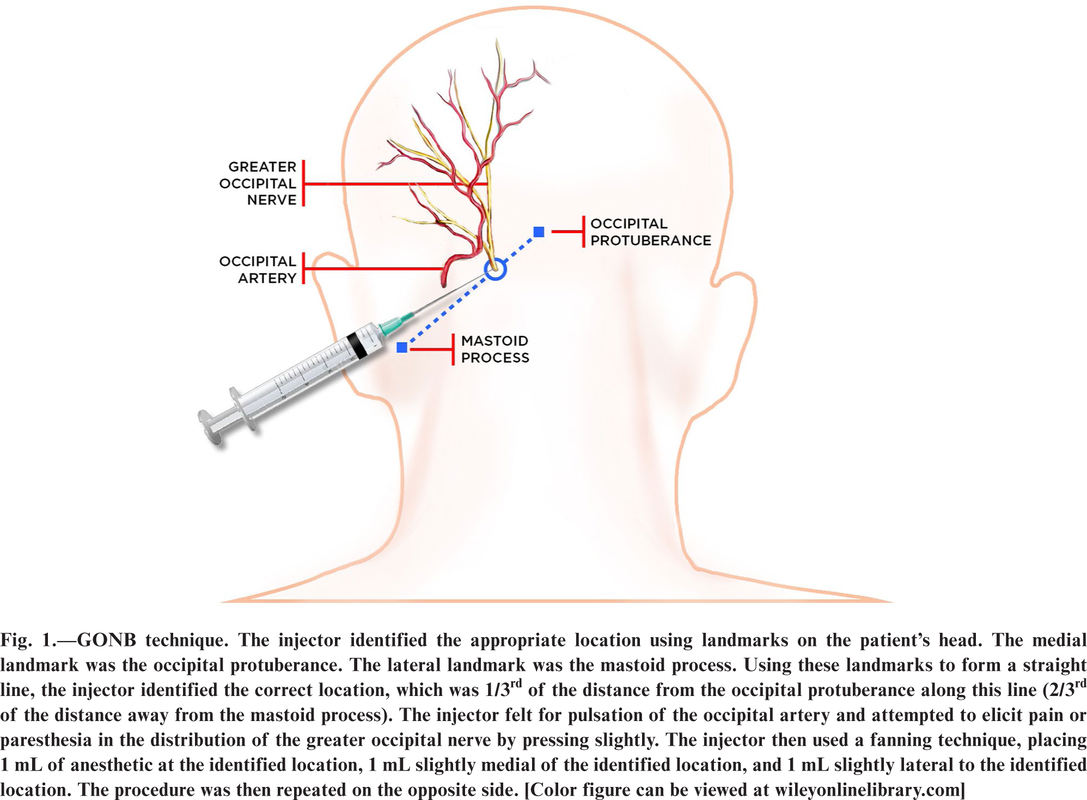
The greater occipital nerve is localized as the point at the proximal third of a line from the inion to the mastoid process.
Needle enters skin at red dot and is inserted along the red line toward the inion and then pulled back to ensure there is
no blood return. Medication (1.5-3 cc) is then delivered along the red line as the needle is withdrawn. The needle is removed, and the process repeated along the red line in the opposite direction toward the mastoid, delivering another 1.5-3 cc of medication.
Friedman BW, Irizarry E, Williams A, Solorzano C, Zias E, Robbins MS, Harrilal MA, Del Valle M, Bijur PE, Gallagher EJ. A Randomized, Double-Dummy, Emergency Department-Based Study of Greater Occipital Nerve Block With Bupivacaine vs Intravenous Metoclopramide for Treatment of Migraine. Headache. 2020 Nov;60(10):2380-2388. doi: 10.1111/head.13961. Epub 2020 Sep 27. PMID: 32981043; PMCID: PMC7704709.
Occipital Nerve Block - Alternative (Andrew Blumenfeld)
- 0.5% marcaine
- 27 gauge needle, 1 inch
- Inject both greater and lesser occipital nerves (1 cc each) - advance to periosteum, pull back to check blood flush
- Injection sites: either side of midpoint between inion (external occipital protuberance) and mastoid process; alternatively 1/3rd from inion and 1/3rd from mastoid
- 3rd injection suboccipital 0.5 cc - don't hit periosteum
- 3 separate injections, raise welt
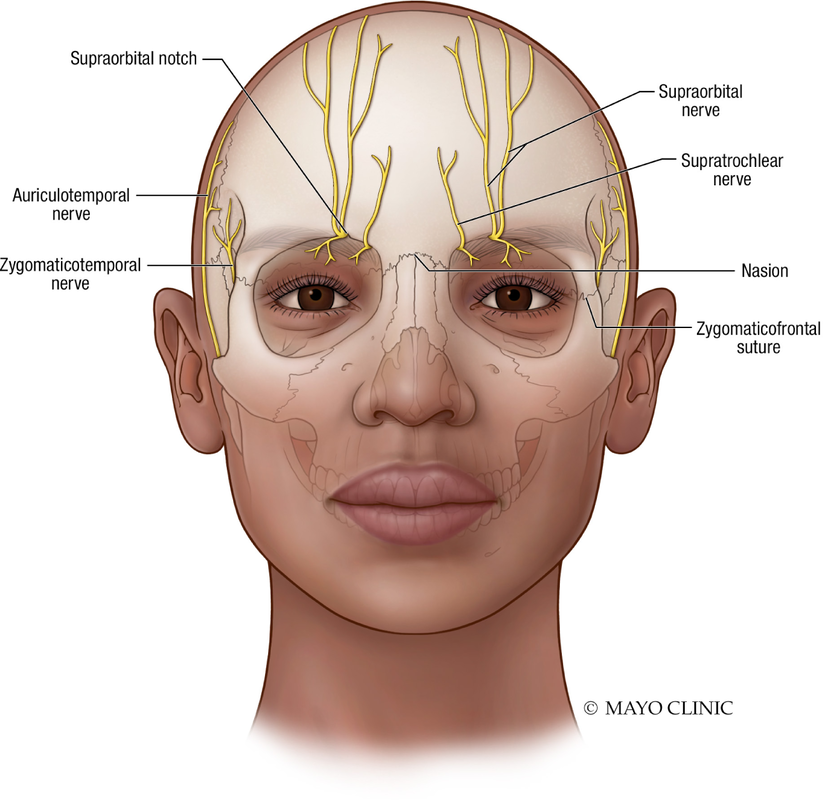
Supraorbital and Supratrochlear Nerve Blocks
Supra Orbital Nerve Block video ---> youtu.be/RXy5SwDn9nw
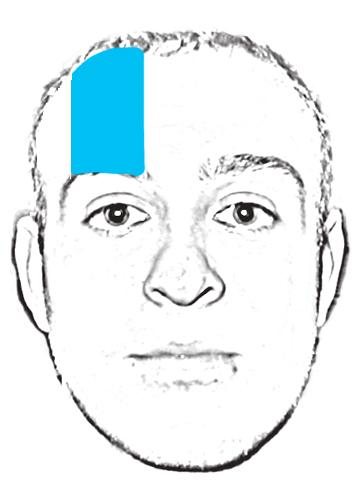
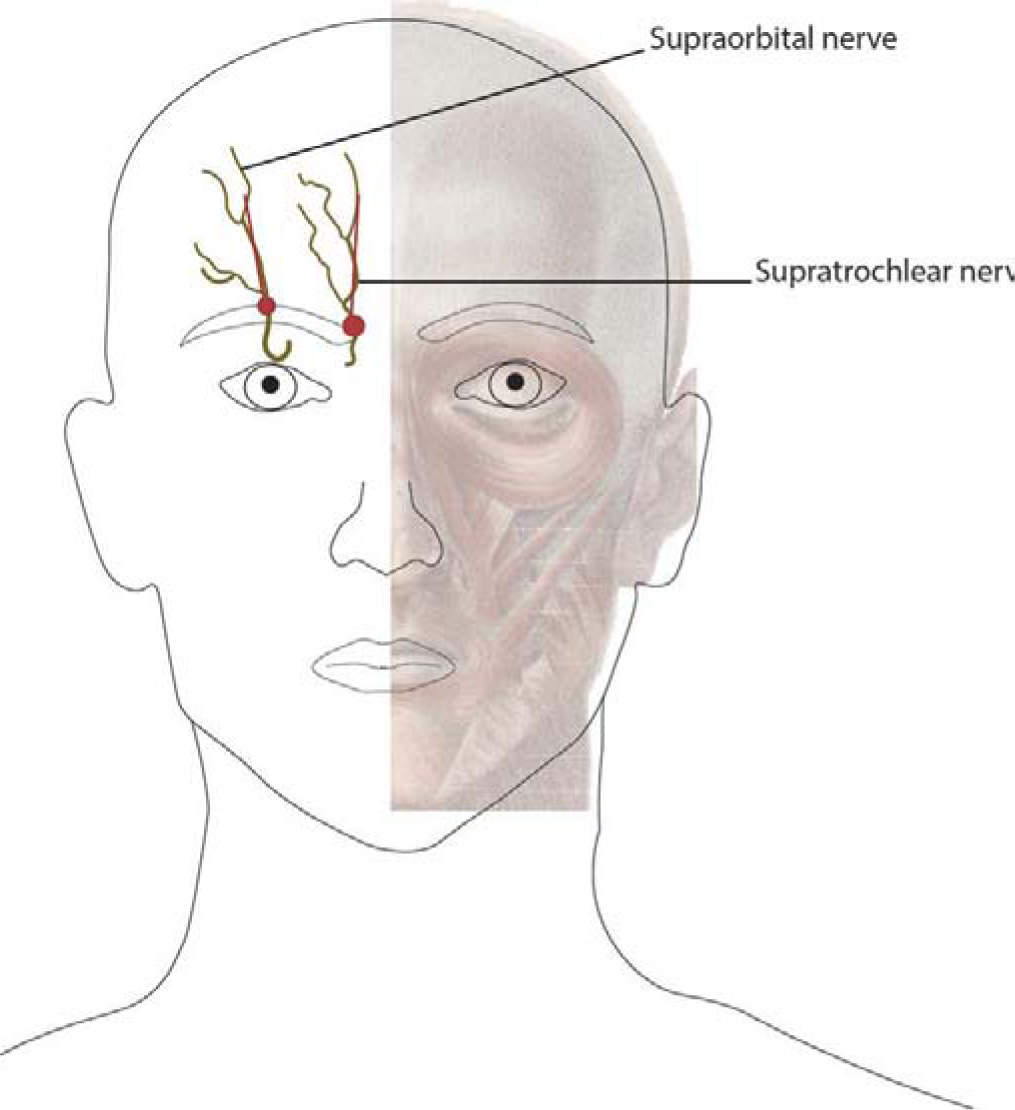
To localize the supraorbital or supratrochlear nerve, the supraorbital ridge is identified by palpation and the site of needle insertion is superior to the ridge.
Using direct palpation, the supraorbital foramen is identified and the needle is inserted into the red dots (superomedial corner of the orbit for supratrochlear nerve and the mid-pupillary line for the supraorbital nerve) infiltrating in the areas of supraorbital and supratrochlear nerves and being careful to remain superficial throughout the entire process.
Luer-Lok syringe, 3 mL Needle, 25-27 gauge (ga), 1.5 in
The supraorbital nerve exits the supraorbital foramen, which lies approximately 2-3 cm lateral to the midline of the face, at the inferior edge of the supraorbital ridge.
To locate the supraorbital foramen, have the patient look straight ahead and imagine a line drawn vertically (sagittally) from the pupil up toward the inferior border of the supraorbital ridge. Then palpate along the supraorbital ridge until a subtle notch is felt; this is the supraorbital foramen. See image below.
Complications: Bleeding, Hematoma formation, Allergic or systemic reaction to anesthetic agent, Infection, Unintentional injection into artery or vein, Failure to anesthetize, Nerve damage, Swelling of the eyelid
Using direct palpation, the supraorbital foramen is identified and the needle is inserted into the red dots (superomedial corner of the orbit for supratrochlear nerve and the mid-pupillary line for the supraorbital nerve) infiltrating in the areas of supraorbital and supratrochlear nerves and being careful to remain superficial throughout the entire process.
Luer-Lok syringe, 3 mL Needle, 25-27 gauge (ga), 1.5 in
The supraorbital nerve exits the supraorbital foramen, which lies approximately 2-3 cm lateral to the midline of the face, at the inferior edge of the supraorbital ridge.
To locate the supraorbital foramen, have the patient look straight ahead and imagine a line drawn vertically (sagittally) from the pupil up toward the inferior border of the supraorbital ridge. Then palpate along the supraorbital ridge until a subtle notch is felt; this is the supraorbital foramen. See image below.
Complications: Bleeding, Hematoma formation, Allergic or systemic reaction to anesthetic agent, Infection, Unintentional injection into artery or vein, Failure to anesthetize, Nerve damage, Swelling of the eyelid
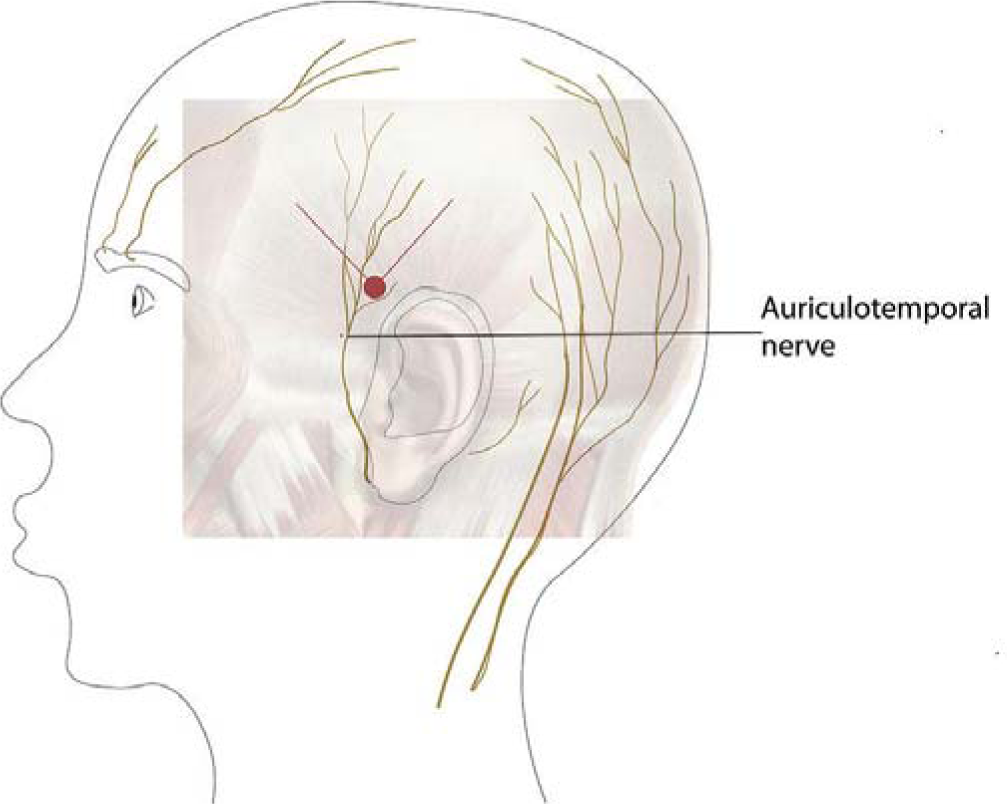
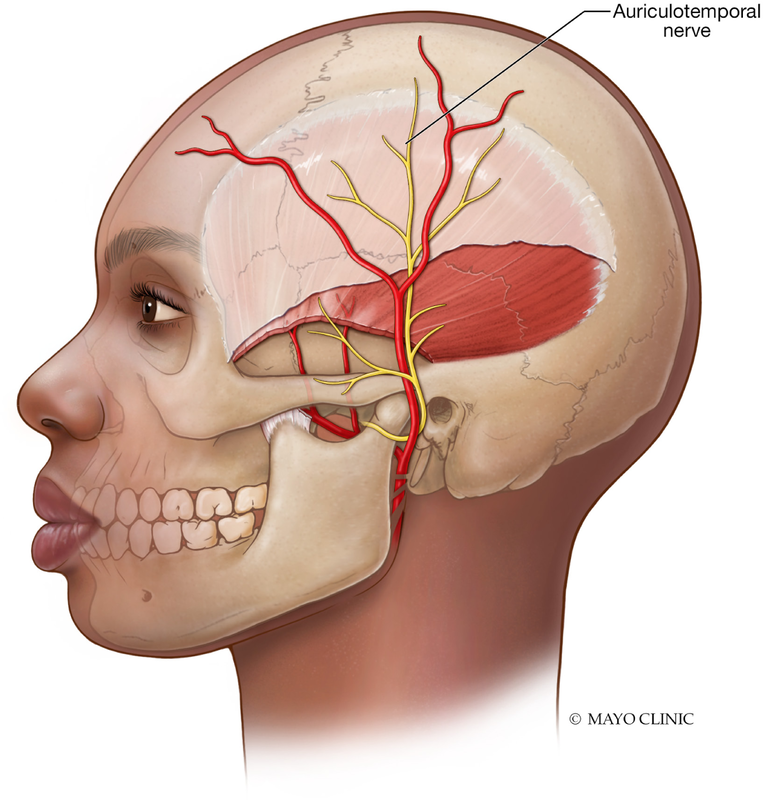
Auriculotemporal Nerve Block
The auriculotemporal nerve is localized by palpating the temporal artery at the level of the tragus and moving 2 fingerbreadths anterior and superior
Using direct palpation, the temporal artery pulse is located, and the skin prepared with alcohol. Next, the needle is inserted into the red dot (anterior to the temporal artery above the posterior part of the zygoma) infiltrating in the area of the auriculotemporal nerve and again being careful to remain superficial throughout the entire process.
Using direct palpation, the temporal artery pulse is located, and the skin prepared with alcohol. Next, the needle is inserted into the red dot (anterior to the temporal artery above the posterior part of the zygoma) infiltrating in the area of the auriculotemporal nerve and again being careful to remain superficial throughout the entire process.
Sphenopalatine Ganglion Block
Sphenopalatine ganglion (SPG) blockade can be achieved with various approaches. The least invasive is the intranasal administration of anesthetic to the nasal mucosa vs a more invasive injection through the cheek with fluoroscopic guidance. Traditionally the procedure was performed with a cotton-tipped applicator immersed in a concentrated local anesthetic, such as lidocaine, 4%, and applied to the posterolateral wall of the nasal cavity. The patient is positioned supine and the head turned toward the side of application during insertion of the anesthetic.17 Simpler methods now exist with the use of devices that allow for a small, flexible catheter to be advanced into the nasal cavity and delivery of local anesthetic, such as bupivacaine, 0.5%, to the posterolateral wall of the nasal cavity. This technique not only allows the patient to remain upright for the procedure but also takes less time to administer and results in less discomfort.