Diagnosing Dizziness - Vestibular Migraine: Duration and Triggers are key
Duration
Triggers
- Seconds: vestibular paroxysmia, bow hunter syndrome (rotational vertebral artery syndrome), arrhythmia
- Seconds to minutes: BPPV
- Minutes to hours: TIA, Meniere’s
- Minutes to days: migraine
- Days: vestibular neuritis (peripheral), stroke (central) – Important: use HINTS plus to rule out stroke
- Months and longer: persistent postural perceptual dizziness, mal debarquement, psychogenic
Triggers
- Turning in bed, reaching overhead: BPPV
- Rising to upright position: orthostatic, POTS
- Neck turning: Bow hunter’s syndrome (rotational vertebral artery syndrome), vestibular paroxysmia (analog of trigeminal neuralgia), Chiari malformation
- Travel: Mal debebarquement (at sea, haven’t lost sea(worse when still in bed, better while moving)
- Loud noises, straining: abnormal connectivity between middle and inner ear
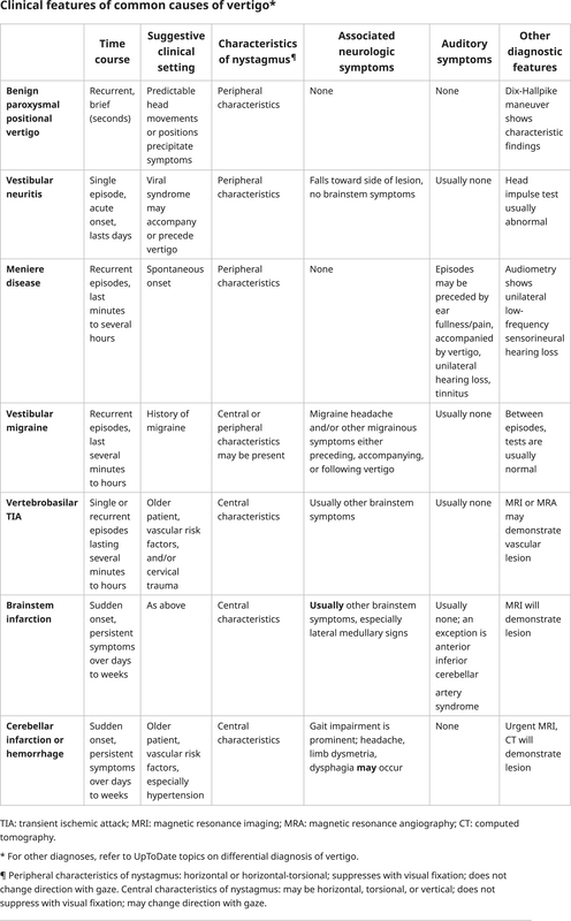
Clinical Features of Vertigo
Differential Diagnosis of Vertigo
The differential diagnosis in patients presenting with vertigo can be broken down to that of peripheral or central etiologies as well as those with or without hearing loss:
Peripheral Causes:
Benign paroxysmal positional vertigo (BPPV): Presents with episodic vertigo following predictable head movements that trigger symptoms. It is usually an acute onset with a duration of seconds to minutes.
Meniere disease: Presents acutely with recurrent episodes of vertigo along with sensory symptoms (e.g., ear fullness, tinnitus, low-frequency hearing loss). Symptoms last minutes to hours.
Labyrinthitis: Presents with similar symptoms to vestibular neuritis but will also include auditory symptoms such as unilateral hearing loss. Symptom duration lasts days to weeks.
Central Causes:
Vestibular migraine: Can present with central or peripheral signs/symptoms. Patients will have a headache and will note recurrent episodes and must have a documented diagnosis of migraine. Symptoms duration is minutes to hours.
Vertebrobasilar TIA: Patients will usually have vascular risk factors. Symptoms are shorter and of acute onset. Symptoms duration is minutes to hours
Brainstem ischemia/infarct: Patients will often have vascular risk factors or a history of trauma. There is commonly noted to be a constellation of neurological symptoms along with vertigo present, known as a Wallenberg syndrome, which is an infarct of the lateral medulla. The onset is acute, and the duration of symptoms is days to weeks.
Cerebellar infarct or hemorrhage - There are usually vascular risk factors or trauma present. Symptom onset is acute, and the duration is days to weeks. There are typically associated neurological deficits present along with an abnormal HINTS exam, truncal instability, headache, ipsilateral Horner syndrome, limb ataxia, abnormal pupillary response, and other neurological abnormalities.
Hearing Loss Present:
Peripheral Causes:
Benign paroxysmal positional vertigo (BPPV): Presents with episodic vertigo following predictable head movements that trigger symptoms. It is usually an acute onset with a duration of seconds to minutes.
Meniere disease: Presents acutely with recurrent episodes of vertigo along with sensory symptoms (e.g., ear fullness, tinnitus, low-frequency hearing loss). Symptoms last minutes to hours.
Labyrinthitis: Presents with similar symptoms to vestibular neuritis but will also include auditory symptoms such as unilateral hearing loss. Symptom duration lasts days to weeks.
Central Causes:
Vestibular migraine: Can present with central or peripheral signs/symptoms. Patients will have a headache and will note recurrent episodes and must have a documented diagnosis of migraine. Symptoms duration is minutes to hours.
Vertebrobasilar TIA: Patients will usually have vascular risk factors. Symptoms are shorter and of acute onset. Symptoms duration is minutes to hours
Brainstem ischemia/infarct: Patients will often have vascular risk factors or a history of trauma. There is commonly noted to be a constellation of neurological symptoms along with vertigo present, known as a Wallenberg syndrome, which is an infarct of the lateral medulla. The onset is acute, and the duration of symptoms is days to weeks.
Cerebellar infarct or hemorrhage - There are usually vascular risk factors or trauma present. Symptom onset is acute, and the duration is days to weeks. There are typically associated neurological deficits present along with an abnormal HINTS exam, truncal instability, headache, ipsilateral Horner syndrome, limb ataxia, abnormal pupillary response, and other neurological abnormalities.
Hearing Loss Present:
- Perilymphatic fistula
- Cholesteatoma
- Meniere disease
- Labyrinthitis
- Acoustic neuroma
- Autoimmune processes
- Psychogenic
- Benign positional paroxysmal vertigo
- Vertebral basilar insufficiency
- Migraines
- Vestibulopathy
- Vestibular neuronitis
- Central nervous system disorders
- Lyme disease
- Multiple sclerosis
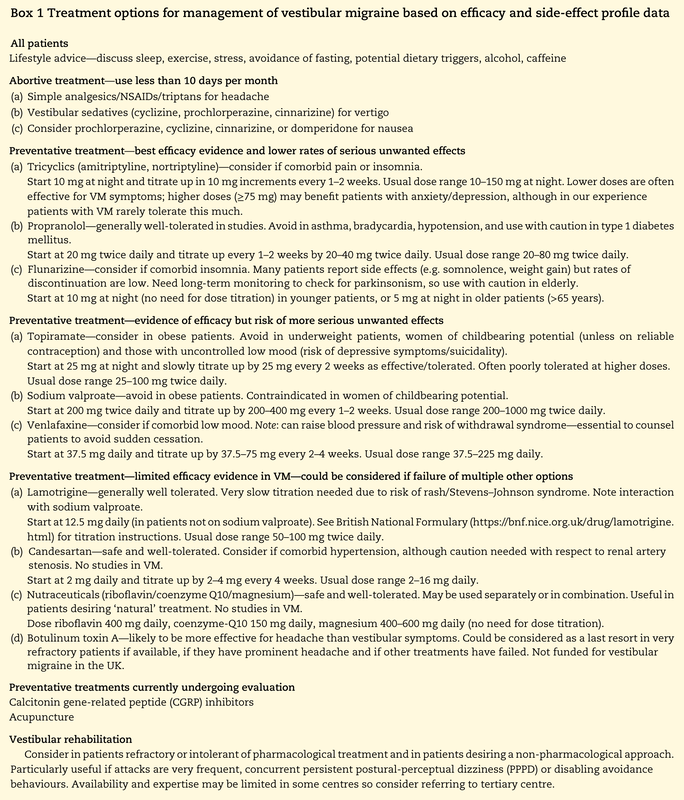
Vestibular Migraine Treatment
Smyth D, Britton Z, Murdin L, Arshad Q, Kaski D. Vestibular migraine treatment: a comprehensive practical review. Brain. 2022 Nov 21;145(11):3741-3754. doi: 10.1093/brain/awac264. PMID: 35859353; PMCID: PMC9679161. Download here.
Testing UC Davis ENT
- Hearing Evaluation
- Electronystagmography/Videonystagmography (VNG): ENG records eye movements using either electrodes placed under eyes or VNG goggles with small video cameras
- Vestibular Evoked Myogenic Potentials: surface electrodes on neck and face to evaluate the muscle responses and neural pathways which connect to the vestibular system.
- Video Head Impulse Test: video gogles measure eye movements when head is turned from left to right and up and down.
Clinic Findings in Vestibular Migraine
- Cannot tolerate OKN
- Imperfect smooth pursuit in young patients
Acute Attacks of Vestibular Migraine
Vestibular suppressants can be used to treat acute attacks of vestibular migraine that last more than 20 to 30 minutes when the vertigo or nausea are significant.
- Benzodiazepines (diazepam, lorazepam)
- Antiemetics (promethazine)
- Antihistamines (meclizine, dimenhydrinate); rectal if vomiting prevents.
- Triptans not routinely used for acute attacks of vestibular migraine; may be considered when headache symptoms accompany vertigo attacks or when vertigo acts as a migraine aura. Some studies indicate efficacy in vestibular migraine.
Preventive Treatment of Vestibular Migraine
- Avoid triggers
- Beta blockers, tricyclic antidepressants, or topiramate when treating both episodic vertigo and headaches.
- Venlafaxine when vestibular symptoms predominate (especially with comorbid persistent postural-perceptual dizziness [PPPD], anxiety, or depression), recognizing that SNRIs can sometimes worsen headaches.
- Verapamil in the uncommon situation where vertigo acts as a migraine aura or other aura symptoms are prominent.
What is Vertigo (in BPPV)?
- Illusory sensation of motion of either the self or the surroundings.
- Symptoms of vertigo resulting from posterior canal BPPV are typically described as a rotational or spinning sensation when the patient changes head position relative to gravity.
- Episodes often provoked by everyday activities and commonly occur when rolling over in bed or when the patient is tilting the head to look upward (eg, to place an object on a shelf higher than the head) or bending forward (eg, to tie shoes).
Dix-Hallpike Maneuver
Procedure:
- Make the patient sit on examination table, such that the shoulders would level on the edge of table when lying down
- Always start the examination with the ear that is least suspected
- Turn the patient’s head to 45° towards the test ear, by holding the both sides of the patient’s head with your hands
- Instruct the patient to fix his/her eyes on a point directly in front of him/her and keep the eyes open throughout the test
- Supports the patient’s head as the patient lies back quickly from a sitting to supine position, ending with the head hanging 30 degrees off the end of the examination table
- Observe (nystagmus, vertiginous symptoms) the patient in this position for 30 seconds
- Then the patient returns to the upright position and is observed* for 30 seconds.
- Repeat the entire maneuver with the head turned 45 degrees toward the opposite side.
- Observe (nystagmus, vertiginous symptoms)
- When the head is lowered 30 degree below the bed, the fast phase of the nystagmus is upward, rotating toward the affected ear
- When the patient is brought back to the sitting position, the fast phase of the nystagmus is downward, rotating toward the affected ear
Vestibular Neuronitis
The typical presentation of vestibular neuritis is usually with the acute onset of the following:
Other symptoms, such as headaches, are usually absent. It is vital to ask the patient about accompanying symptoms that may suggest central disorders of vertigo, such as visual changes, somatosensory changes, weakness, dysarthria, incoordination, or an inability to walk. If any of these are present, one must broaden the differential with to central causes of vertigo. When the additional symptom of unilateral hearing loss is present, this shifts the diagnosis towards labyrinthitis. When attempting to differentiate this associated hearing change from Meniere disease, it is important to know that Meniere disease also presents with vestibular and auditory dysfunction. Still, patients with Meniere have more episodic and not continuous symptoms lasting 20 minutes to usually no more than 12 hours.
- Vertigo
- Nausea
- Vomiting
- Balance problems
Other symptoms, such as headaches, are usually absent. It is vital to ask the patient about accompanying symptoms that may suggest central disorders of vertigo, such as visual changes, somatosensory changes, weakness, dysarthria, incoordination, or an inability to walk. If any of these are present, one must broaden the differential with to central causes of vertigo. When the additional symptom of unilateral hearing loss is present, this shifts the diagnosis towards labyrinthitis. When attempting to differentiate this associated hearing change from Meniere disease, it is important to know that Meniere disease also presents with vestibular and auditory dysfunction. Still, patients with Meniere have more episodic and not continuous symptoms lasting 20 minutes to usually no more than 12 hours.